What is the connection between biofilms and persistent infections?
Increasing evidence shows that bacteria and yeast can adhere to implanted medical devices or damaged tissue and become the focus of persistent infections (Costerton et al, 1999). Microbial biofilms that form in the human body share certain characteristics with biofilms that are familiar in other environments (see Table 7-1, below; for basic information about biofilm formation, please refer to “Module 1: Introduction to Biofilms” ). Some well-established examples of biofilm infections include cystic fibrosis pneumonia, periodontitis, and infection of catheters and prosthetic joints.
| CHARACTERISTIC | CYSTIC FIBROSIS | PERIODONTITIS | CENTRAL VENOUS CATHETER INFECTION | CHRONIC WOUNDS |
| Form preferentially on foreign bodies, dead or damaged tissue | The genetic defect in the chloride ion channel predisposes the lung to infection | The tooth surface is not as well-defended as are vascularized tissues | Indwelling plastic and metal surfaces are very vulnerable to microbial colonization | Necrotic tissue could provide nidus for biofilm formation |
| Slow to develop | Persistent infection takes years to establish | Typically manifests gradually, later in life | Symptoms may take weeks to manifest | Symptoms such as pain, exudate and size wax and wane over weeks to months |
| Respond poorly or only temporarily to antibiotics | Lung is never cleared of bacteria despite aggressive chemotherapy | Tetracycline, antiseptic mouthwashes have little efficacy | Preferred therapy is removal of the infected catheter | Marginal response to antibiotics; may deteriorate when antibiotics are stopped |
| Collateral damage to neighboring healthy tissue | Massive neutrophil invasion contributes to gradual loss of lung function | Host responses and bacterial virulence factors lead to progressive bone loss; teeth fall out | Infection may disseminate to blood and other locations in body | Normal healing process of cell differentiation and migration is arrested |
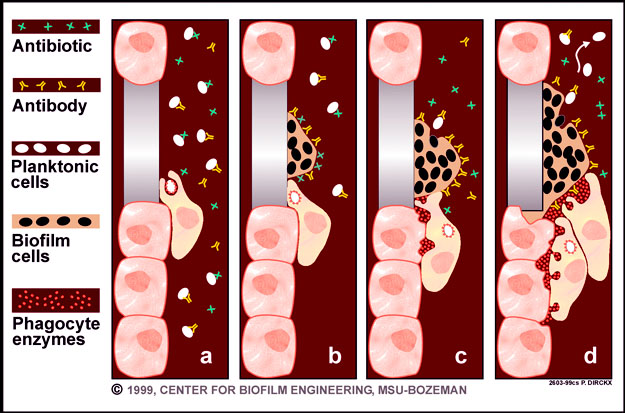
Biofilm infections form preferentially on foreign surfaces as well as dead or damaged tissue. These infections develop gradually and may be slow to produce overt symptoms. Once established, however, biofilm infections persist. They are rarely resolved by host defense mechanisms, even in individuals with healthy innate and adaptive immune reactions. Active host responses, such as invading neutrophils, can even be detrimental since those cells can cause collateral damage to neighboring healthy host tissue. Biofilm infections respond only transiently to antibiotic therapy.